
Winds of Change – One Puffer at a Time
by Dr Monica Theron
MBChB, ClinDipPallMed, FRACGP and FASLM
Short wind, the topic of our Shared Medical Appointment in Mparntwe/Alice Springs.
We talk about short wind causes. Heart troubles. Sick kidneys and missing dialysis. Spirit no good – getting upset or sad. And, short wind from the lungs. But the lungs? Often last on the list at a GP consult.
We prescribe pressured metered-dose inhalers (pMDIs) out of habit. They are familiar and effective. Widely used and may need a spacer. However, their environmental impact is significant and hidden.

The new Asthma handbook 2025 guidelines recommend anti-inflammatory relievers (AIR) or maintenance and reliever therapy (MART) with inhaled corticosteroids (ICS), moving away from “blue puffer” only treatment for adolescents and adults. This aligns with global best practice to improve control, reduce oral steroids reliance and fewer severe attacks[5]. Acknowledging New-Zealand’s approach as DPI’s preferred first line treatment for adult and adolescent asthma[6].
We have the power to reduce carbon emissions from inhalers by up to 90%. A petrol car from Naarm/Melbourne to Central Australia emits the equivalent of 452 dry powder or soft mist inhalers. Not a mere 8 – 13 pressured MDIs.

The greenhouse gas propellants from pMDI’s can continue to leak into the atmosphere if not discarded appropriately. Empty and unwanted inhalers can be taken to pharmacies for safe disposal free of charge. The puffer’s plastic case may be suitable for the household recycling bin[7].
This is not about doing more; it’s about prescribing with intention. A strength-based approach that values clinical care and planetary health. Another tool in the toolkit to augment the unofficial 7th Lifestyle Medicine pillar Nature.
Let’s change the winds together, one puffer at a time.
The Project
A clinical audit in Northern Territory’s largest Aboriginal Community Controlled Health Organisation consisting of town and remote clinics to encourage prescribers to consider prescribing environmentally friendly inhalers in adults.
Objectives
- Implement the intervention in routine practice
- Compare inhaler prescribing rates pre- and post-intervention
- Gather prescriber feedback
- Explore patient-related factors
Simple tools and clinical prompts that make sustainable prescribing easier.
I am hopeful that this wind of insight translates into action – guiding sustainable inhaler prescribing across Central Australia, from town clinics to remote communities
We welcome collaboration on this project; feel free to reach out to Monica on monica.theron@caac.org.au.
- National Institute for Health and Care Excellence (NICE). “Asthma: diagnosis, monitoring and chronic asthma management (NG245).” 2024. https://www.nice.org.uk/guidance/ng245 (accessed 7 Dec 2025)
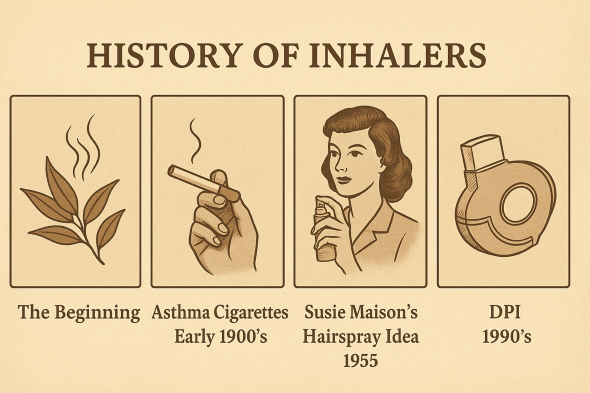
- Stein SW, Thiel CG. “The History of Therapeutic Aerosols: A Chronological Review.” J Aerosol Med Pulm Drug Deliv.2017;30(1):20-41. doi:10.1089/jamp.2016.1297.
- Asthma Australia. “The National Sustainable Asthma Care Roadmap – Roundtable Report.” 2024. https://asthma.org.au/about-us/advocacy/the-national-sustainable-asthma-care-roadmap/ (accessed 7 Dec 2025)
- D Rigby. “Inhaler device selection for people with asthma or chronic obstructive pulmonary disease.” Aust Prescr.2024;47:140-147. doi:10.18773/austprescr.2024.046.
- Asthma Australia. “Asthma Digest – AAH Update 2025.” 2025. https://asthma.org.au/health-professionals/asthma-digest/aah-update-2025/ (accessed 7 Dec 2025)
- Asthma Foundation New Zealand. “The environmental impact of inhalers.” 2025. https://www.asthmafoundation.org.nz/stories/the-environmental-impact-of-inhalers (accessed 7 Dec 2025)
- National Asthma Council Australia. “Puffer and inhaler care – Factsheet.” 2025. https://files.nationalasthma.org.au/resources/Puffer-and-inhaler-care_-Factsheet.pdf (accessed 7 Dec 2025)

Dr Monica Theron
Monica is a General Practitioner with special interests in Indigenous health, lifestyle medicine and palliative care. She is a Fellow of the Australasian Society of Lifestyle Medicine and a Fellow of Royal Australian College of General Practitioners. Alice Springs NT has been home for the past eight years, providing unique opportunities to work with diverse health organisations including Central Australian Aboriginal Congress and Western Desert Nganampa Walytja Palyantjaku Tjutaku Aboriginal Corporation (Purple House) in Mparntwe/Alice Springs, NT.

