Post card from Milingimbi and the Northern Territory Shared Medical Appointment Project


Background
The Northern Territory Primary Health Network (NTPHN) engaged, me, Associate Professor John Stevens from Southern Cross University (SCU) National Centre for Naturopathic Medicine (NCNM) and the Australasian Society of Lifestyle Medicine (ASLM) to undertake a proof-of-concept trial. John and his colleagues Prof Bob Morgan (ASLM) and Adjunct Prof Garry Egger (NCNM SCU) have been pioneering the use of Shared Medical Appointments (SMAs) for over a decade now and have recently been joined by Ms Kelly Kerin (AMSANT) in this pursuit.
SMAs are individual medical consultations carried out in a group of patients. SMAs are not only a process to delivery medical consultations but are also an enduring, Aboriginal and Torres Strait Islander model of care that brings together groups of people (8-15 or so) with similar concerns, managed by a trusted facilitator who can communicate in language, with their healer, a GP or other clinician. In addition, others in the group are listening, sharing and encouraged to contribute their knowledge and experiences.


There are over 9k peer reviewed papers in the literature supporting the use of SMAs in various health care settings including within Aboriginal communities. SMAs appear to improve cultural safety, responsiveness and accessibility.
The NTPHN proof of concept project aims to see if SMAs can 1) de-colonise the current methods of health service delivery by providing a safe, responsive and accessible model of engagement with Aboriginal people and their communities of the Northern Territory. And, 2) be integrated sustainably into Aboriginal Health Services.
The project involves engaging with Aboriginal communities, health service clinicians and health service managers in the SMA process and then customising the conversations and explanations with Traditional Owners and community members in a continuous co-design process that empowers the community. As well the project provides training for health service clinicians, including Aboriginal Health Practitioners and managers.
This proof of concept project is currently being undertaken over 2 years with the following organisations and the communities they serve; 1) Central Australian Aboriginal Congress Health Service, Alice Springs and related remote communities, 2) Danila Dilba Health Service, Darwin and 3) Miwatj Aboriginal Health Corporation East Arnhem Land.
Mili in the spotlight
Milingimbi is a remote small island (10x 11 KM2) accessible by air (rarely by sea for Balunda) of approximately 1500 people, most of whom are Yolngu. The population lives in a number of established ‘camp’ locations, the equivalent of small urban suburbs. The main language spoken is Yolngu Matha. For most, English is a second or third language with many people not speaking it at all. School is taught to year 11 and education is delivered bilingually. Health issues are vast and representative of other Aboriginal communities in East Arnhem Land. There was an estimate by the clinical staff that about 40-50% of the adult population had Type 2 Diabetes for example.


The community is serviced by one retail shop where all food, clothing and household items are sold. The shop is stocked by a barge from Darwin which delivers fresh food and other items once per week when the tides and weather allow.



Health Services
The main western health service for the community is the Milingimbi Health Clinic, managed by Miwatj Health Aboriginal Corporation. The Clinic provides primary health services and is the hub for a range of visiting specialist services. The clinic also provides emergency services including retrieval to Darwin or Gove hospitals.

Medical Dhawu Dhawu Activity and Outcomes from this visit
Miwatj is one of the organisations participating the proof of concept trial of Shared Medical Appointments (known in Yolngu Matha as Medical Dhäwu Dhäwu). To date, the communities serviced by Miwatj including Nhulunbuy, Yirrkala, Gapuwiyak and Galiwinku have also participated in the MDD activities.


‘It’s all about relationships’
One of the personal highlights of the trip was the development of a relationship with a local trainee Aboriginal Health Practitioner. Tristen provided great insight to ways of localising the MDD process, especially for the men.
I visited and yarned with some of the Traditional Owner (TO) men and Tristen offered to translate for us. My first visit was to pay respect and also ask permission to be able to conduct this work on their Country. The TOs provided permission and also valuable feedback on the MDD process when it was explained to them. They unanimously advised us that if it worked like they thought it might, MDD would be a preferred way of seeing the Doctor and other clinic staff for non-urgent, ongoing health issues (this included chronic illness management according to Tristen’s translation.)
A number of the TOs asked the MDD team to come to a Learning On Country session to see what health education they were already providing to their younger men and to exchange ideas on health with them.
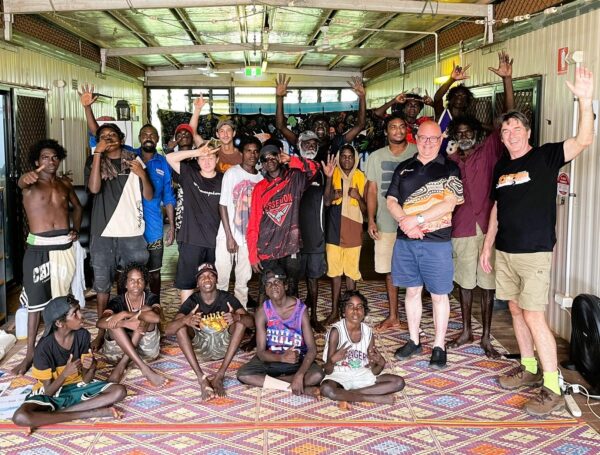
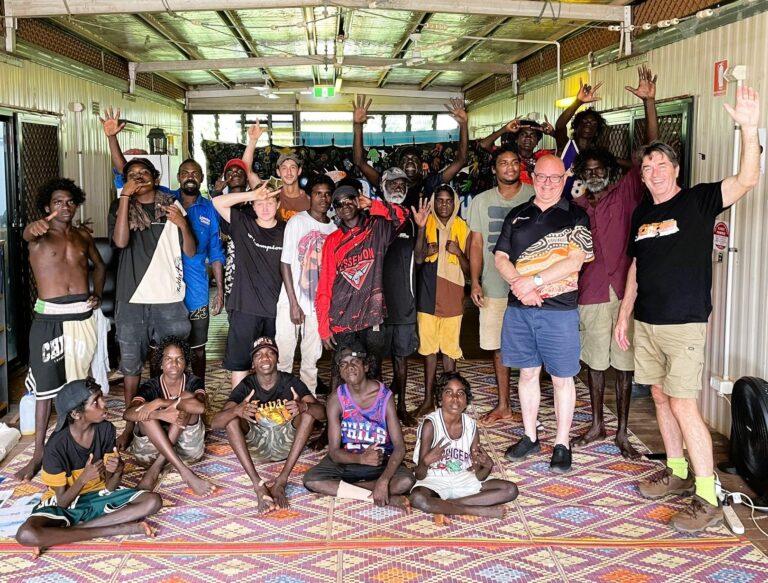
Dr Steve (Miwatj GP), Tristen and I attended a men and boys Learning On Country session the next day. Learning on Country provides the opportunity for the elder men and knowledge keepers to mentor youth in traditional ways and culture. They day we visited the older men were teaching the younger how to collect and prepare bush medicine that had been part of the their science for thousands of years.
Dr Steve and I explained, with the help of Tristan’s interpreting, the MDD process that the clinic would like to establish. Our yarn with the Learning On Country group was well received. We were then invited by the relevant TOs to visit all of the island camps over the following weeks to undertake MDD. Tristen and Dr Steve have subsequently developed a plan to visit the camps each Wednesday over the next 4 weeks of Dr Steve’s rotation on the Island.

One of those visits occurred the following day. The TO provided verbal permission for me to report on our experience. Led by Tristan, Dr Steve and I sat on the ground with eight men and two boys in a circle under their lean-to and began the island’s first MDD. The main aim of this MDD was to establish a relationship between Dr Steve and the men of the camp and get a feeling for the process.
The men explained some of their issues at the camp. One major ongoing problem, common to the entire Island community was expressed, regarding the difficulty in obtaining ‘good’ food from the shop. Nutritious food is expensive, (the author visited the shop on arrival and noted on the 30th April 2024: an iceberg lettuce@ $8, apples@ $7kg, 750 ml bottle of Olive oil@ $22, 1kg rice @ $7, potatoes @ $7kg, Frozen rump steak @ $50kg, 2L Cola @ $4, Single serve Asian noodles .60c/per packet) the variety of food was limited).
The men said that the shop could be difficult to access. The camp for example, was approximately 4.5 km away. Roads were often impassable during wet season to people on foot or in vehicles. Indeed, the day we visited the camp, the shop was shut the entire day for stocktake. There was no other way to purchase food on the island while the shop was shut. The men reported people went hungry that day because they did not know of the closure.
The men explained how they used hunting to help them stay healthy, as it gave them bush food, exercise and kept the young engaged in culture. They were keen to tell us about some of their bush medicines.
The men were also keen to explore the MDD concept and said clearly, that they wanted to exchange knowledge not just receive it and this might be a way to do it. They shared stories with us of ill health from diabetes and kidney disease that they believed were healed by hunting. Though they knew plenty of people on the island that needed more help than would come from hunting and that’s why they were interest in MDD.
They told us stories about how they hadn’t been healthy at times because of drinking too much Kava. One man asked specifically about the dangers of Kava which Dr Steve was able to answer. The men then wanted to hear stories from us about our personal issues, had we engaged behaviours that were unhealthy? Dr Steve and I both provided stories of our past that recalled unhealthy eating, drinking and smoking behaviours. The honest exchange of stories was important part of the MDD process for people on Mili.
One man presented a boil on his upper right leg to Dr Steve, and it was used as a teaching opportunity to help explain that boils were the result of ‘germs’ and in some people without treatment, those germs could travel by the blood to heart and kidneys.
This was new information for some. Tristen explained that the men did not always conceive the body the way we, as western clinicians, do. The idea of germs travelling through blood causing trouble was novel to some. The men provided us with some insight about their belief systems of the body. I interpreted the explanation, with the help of Tristan translating to mean, that their bodies were part of something bigger and more spiritual and that connection to spirit and Country was determining their health and illness.
The man with the boil was able to navigate both belief systems with the help of Tristan’s translations and thought it a good idea to keep using bush medicines, but also felt it would be good to visit the clinic the following day for additional help from Dr Steve and antibiotics.
By the end of the approximately 60-minute session there was a positive feeling about the MDD exchange. We were all pleased that it had been an exchange of stories and knowledge. The MDD team were able to acknowledge and appreciate the men’s health behaviours and bush medicines. This was ancient knowledge that we were privileged to be shown, and it was respected.
The men were unanimous about how important it was that we had come to sit with them in the camp under their awning. They did not want their photo taken this time but were happy for us to take a photo of the awning we met under (and their pet Brolga, Maurice).

Before we left, the TO told us that no doctor had sat with them like this in the past from his memory. The men were looking forward to developing this method of consulting.
In a debriefing, Dr Steve voiced his appreciation for the experience of his first MDD. Though we had some refining of the process to work on, he could see how it would improve in time and with practice. It was for him, a great exchange and a start to developing MDD in the community.
Dr Steve fed back, that as well as the positive relationship development and the general health yarning that took place, he was able to discern the requirements being met for MBS billable consultations with some of the men during that first MDD.
Tristen was pleased to report that the men spoke very positively about the exchange in language after we left and that they would be telling others in their camp and on the island about the positive experience they had with MDD.
Before the end of that day Tristen was able to ascertain that men at each of the other camps on the island were keen to experience MDD over the next few weeks.
In Summary
The positives: The Milingimbi Clinical staff were so welcoming and could not be more helpful. They were well briefed about MDD and were keen to support a model of care that would further empower the community. During this short visit:
- A large portion of the community became aware of MDD
- Eight men and 2 boys participated in a first men’s MDD
- Traditional owners were made aware of the MDD process and have told us that they like it.
- The MDD team was given permission to undertake MDD at all camps on the Island by the TOs.
- That traditional healing knowledge and science was valued and privileged in our exchanges. According to Tristen, Yolngu refer to this exchange as ‘two ways learning’ and he suggested that little progress will be made if it is not part of the MDD process going forward.
Personal Reflection
It is difficult being a Balanda (Balanda in Yolngu Matha means outsider, non-Indigenous people or Foreigner) who flies in and out of these beautiful but complex and powerful communities to try and gain contextual understanding, confidence and trust to spark an interest in MDD in such a short time. I was touched at how much trust was given in the short duration of my visit by community and clinic staff.
The MDD process can empower the community and I could see that being recognised in every conversation I had and in the one session we ran. There is a desire within community and clinic to make MDD work. The main lessons for me were:
- The time spent in paying respects, developing relationships and understanding with community is not only a requirement of the process and it is simply good manners. Building relationships must occur before any activity begins
- Thinking about a typical primary health care consultation; the current process positions the clinician as the expert and they impart knowledge about health and illness in a one way exchange ‘to’ the patient. This is ludicrous if you consider that Yolngu have been thriving for tens of thousands of years without western medicines and health care. Privileging, respecting and including traditional knowledge that is possibly tens of thousands of years old (we can’t get more evidence-based than that), must become part of the regular exchange with community and health services if the health Gap is ever to close.
The Medical Dhäwu Dhäwu fire is well and truly alight in Milingimbi.

John Stevens
John Stevens RN, PhD, FACN, FASLM, currently leads the discipline of Lifestyle Medicine at Southern Cross University. He is a Medical Sociologist, a 40-year Registered Nurse and works as a consultant to industry on the implementation of models of care that improve the prevention, management and reversal of lifestyle-related chronic illness by supporting healthcare workers to integrate lifestyle medicine into practice. John is a founder and director of the Australasian Society of Lifestyle Medicine (ASLM), which he and his colleagues officially established in 2008. John has been pioneering Shared Medical Appointments (aka Group Consultations and Medical Yarn Ups) in Australia and New Zealand and has been acknowledged by his peers with a Lifestyle Medicine, Outstanding Achievement Award for his contribution to the well-being of the community through this work. John has over 100 published articles in matters relating to Lifestyle Medicine and is regularly invited to speak at conferences and public events. He lives and thrives in the rural town of Mullumbimby, NSW, Australia, with his wife and five children.

