The endothelium and chronic disease
The 0.2-0.3 µm barrier between blood and tissue is where the ‘rubber meets the road’ in Lifestyle Medicine.
The link between lifestyle and chronic disease is now undisputed. But where is the biological connection? We know inactivity, smoking, bad diet etc. all cause heart disease – amongst other nasties. And we know that some risk factors like cholesterol, hypertension and hyperglycaemia, provide a window to what’s going on. But obviously there’s more to it than that.
In the early 1990s, a clue was found when Harvard researchers associated obesity with a form of chronic, low-level systemic inflammation, which they called ‘metaflammation’ because of its link with the metabolic system. This suggested that obesity may need to be re-framed as an inflammatory disease.
However, it wasn’t long before other stimulants came to be associated with metaflammation. Some of these (eg. over-nutrition, inactivity, a high fat diet) can cause weight gain and so the link with obesity seemed proven. It was even possible that this could provide the causal link between obesity and chronic disease such as type 2 diabetes and heart disease.
But things are never as simple as they seem. Around the middle of the first decade of the 21st Century, it became obvious that obesity is not necessary for metaflammation to develop. In some cases this might be stimulated by the causes of obesity, but obesity is not a pre-requisite. There are acute post-prandial rises in markers of inflammation with weight gain, and some metaflammatory stimulants (smoking, pollution, inadequate sleep) don’t require weight gain at all.
Lifestyle it seems, is sufficient to cause an inflammatory reaction. But not just any lifestyle: A greater reaction appears to occur to modern lifestyle behaviours that have arisen since the industrial revolution – inactivity, lack of sleep, stress, smoking, processed foods etc. The body’s immune system it now appears, is programmed to react not just to microbial invasion and injury, as it has done for millions of years, but to the things we do, and don’t do (eg. exercise) – albeit at a lower, but more chronic level.
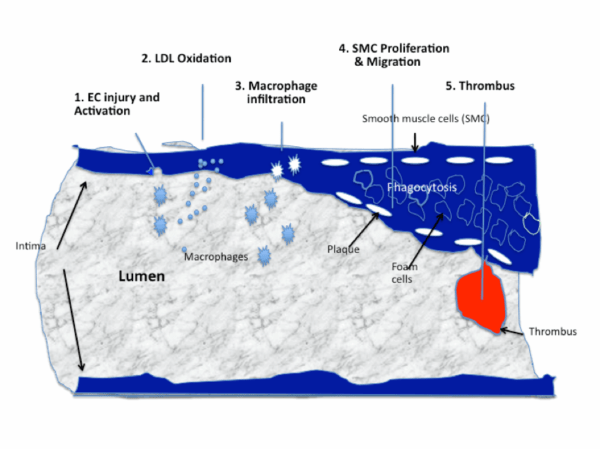
Metaflammation now appears to be the link between lifestyle and many, if not all forms of chronic diseases – including much cancer. Anatomically, the place where this occurs is in the endothelial lining of the blood vessels throughout the body. The endothelium is seems, is where the rubber meets the road in lifestyle related health disorders. Our knowledge to date suggests it happens like this:
- Lifestyle-related ‘inducers’ (eg. a high fat diet, inactivity, smoking etc), incite some physiological ‘agent’ (eg. oxidised LDL cholesterol, particulate matter), which acts like an antigen in the blood;
- This attaches itself to the intimal wall and initiates an immune reaction;
- Macrophages from monocytes in the blood infiltrate the intima and phagocytose the foreign stimuli;
- Foam cells from this process form in the intimal wall causing atheroma;
- Smooth muscle cells form a fibrous cap (plaque) over the occlusive ‘bulge’ into the lumen of the vessel, resulting in chronic atherogenesis;
- If this becomes unstable and bursts, a thrombus can result.
In simple terms, metaflammation thus becomes to chronic disease, what classical information is to injury or microbial invasion. The main difference is that the latter, which is associated with infectious disease, usually leads to a resolution to homeostasis. The former however, leads to dysmetabolism and chronic allostasis (the opposite to homeostasis), and ultimately chronic disease.
This new form of inflammation may explain some of the morbidity/mortality that is not explained by the classical chronic disease risk factors (cholesterol, hypertension, hyperglycaemia etc). How it does this is not yet quite clear, but it seems that metaflammation does have an influence in the development of insulin resistance, probably through blocking insulin signalling in insulin receptors.
Of most significance are the implications for management. Metaflammation can be picked up in inflammatory markers such as hsCRP. As this doesn’t rise to anywhere near the levels associated with acute inflammation however, there may be a tendency to ignore a CRP just 5-6 times the recommended upper level, which could be indicative of metaflammation. This should be taken as a sign that action is needed – but what action?
Reducing obesity has been thought to be the first line of attack. But as suggested above, metaflammation can also result from lifestyle factors that may – or may not – cause obesity. This suggests it would be a mistake to treat obesity like a single lock solution (ie. prescribe just a diet, or just an exercise program). It should be seen more as a barrel lock, where all the barrels (different components of lifestyle) need to be lined up. If this is done, weight loss is likely to result anyway.
Anti-inflammatories are also an obvious line of attack and this possibly explains the well-known benefits of salicylates in heart disease. However, these are likely to have only palliative value if the main cause of the problem (ie. unhealthy lifestyle) is maintained.
As more is discovered, this new form of inflammation is likely to provide a revealing insight into chronic disease. In the meantime, the complex relationship between inflammation and obesity is making us re-evaluate the relationship with obesity and ill-health. But more on that another time.